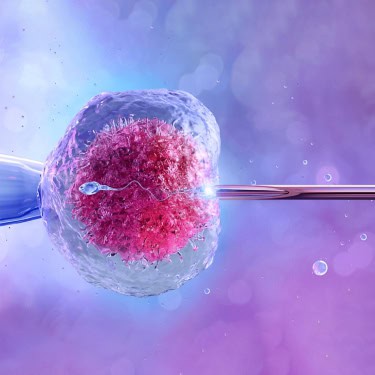
What is IVF (In Vitro Fertilization)?
In Vitro Fertilization (IVF) is a type of assisted reproductive technology. It involves retrieving eggs from a woman's ovaries and fertilizing them with sperm in a specialized laboratory. After fertilizing the eggs, they develop into embryos in a controlled environment for several days. Once they are ready, one or more embryos are transferred to the woman's uterus, increasing the chances of pregnancy.
Why is IVF Treatment Used?
People may turn to IVF for various reasons, including infertility issues or if one partner has a medical condition. It's often an option when other fertility treatments haven't been successful or if the woman is older and past her optimal reproductive age. IVF is also a viable choice for same-sex couples and individuals wanting to become parents.
IVF might be considered if you or your partner has:
- Endometriosis
- Low sperm count or other sperm-related problems
- Blocked or damaged fallopian tubes
- Uterine complications
- Ovarian issues, such as Polycystic Ovary Syndrome (PCOS)
- A risk of transmitting a hereditary illness
- Involvement of a gestational surrogate or egg donor

What are the steps involved in IVF treatment?
Many people hesitate to visit a doctor because of the time it may take. However, this shouldn't stop you. The fertility specialists at the clinic can guide you through the complexities of conceiving with IVF. If you're interested in understanding the steps involved in IVF treatment, we've provided a detailed outline of the procedure below:
Step 1: Doctor Consultation
The consultation may involve three stages, depending on your needs:
- Initial Meeting: The doctor will review your and your partner's medical histories. It's essential to be open and honest during this discussion. Based on this assessment, they will recommend an IVF procedure.
- Diagnosis Review: The doctor will provide a diagnosis and discuss whether you need to take stimulation medication yourself.
- Cost Discussion: The doctor will explain the total costs of the IVF procedure.
Step 2: Preparation for the Procedure
During this stage, you will need to complete several pre-IVF tests, including:
- Blood tests
- Male fertility testing, such as semen analysis
- Ultrasound
- Infectious disease screening
- Uterine evaluation
These tests provide a comprehensive overview of your health and help identify the leading causes of infertility.
Step 3: Medication and Monitoring
You will begin a process known as controlled ovarian hyperstimulation (COH). This starts with an ultrasound to check your ovaries and uterus. Once the doctor confirms everything is in order, the process will continue. COH consists of two essential parts:
- Fertility Medications: You will take fertility medications orally or through injections. These drugs stimulate the ovarian follicles, encouraging more eggs to mature than in a typical cycle, to produce four healthy eggs.
- Monitoring: After the ovaries are stimulated, you'll need to visit the clinic several times to monitor the development of your eggs and follicles. This phase is the most time-intensive, usually requiring 5-7 visits to the doctor's office.
Step 4: Triggering, Egg Retrieval, and Fertilization
The final step involves triggering egg maturation with hCG and scheduling egg retrieval. This process includes four main parts:
- Egg Retrieval: The egg retrieval is performed under sedation. While minimal risks exist, you may want to take a day off work to recover, as the procedure can be tiring.
- Combining Egg and Sperm in the Lab: After the eggs are retrieved, fertilization occurs, leading to the creation of embryos. Various techniques are used to boost the chances of a successful pregnancy:
- Intracytoplasmic Sperm Injection (ICSI): This method benefits male fertility issues. It involves injecting a single healthy sperm directly into the egg.
- Assisted Hatching: A small hole is made in the embryo's outer layer to help improve implantation rates after transfer.
- Preimplantation Genetic Screening: This ensures that only healthy embryos are transferred. It can also be done on frozen embryos.
Step 5: Evaluation of Embryos (3-6 Days After Fertilization)
From the day after fertilization, embryos are monitored daily to determine which ones are healthy enough for transfer.
Step 6: Embryo Transfer
Three days post-fertilization, embryos are ready for transfer. Some patients may wait until the embryos reach the blastocyst stage five days after fertilization. The embryo is transferred using a thin, flexible tube gently passed through the cervix into the uterus. This procedure is painless, though you may feel mild cramps.
Step 7: Pregnancy Test
A blood test is conducted two weeks after the egg retrieval. If the test is positive, you will be considered four weeks pregnant.
Role of Injections in IVF
In IVF, injections are essential, particularly during the ovarian stimulation phase. Hormones such as follicle-stimulating hormone (FSH) and luteinizing hormone (LH) are administered to encourage the development of multiple follicles in the ovaries, each containing a potential egg. This differs from the natural menstrual cycle, where only one egg is typically released each month.
Once the follicles are mature, the next step is to trigger the final maturation of the eggs. This is done with an injection of Human chorionic gonadotropin (hCG), ensuring the eggs are ready for retrieval. The timing of this injection is crucial, as it helps synchronize the reproductive process for a successful IVF outcome.
After the eggs are retrieved, injections remain essential for preparing the uterine lining for embryo implantation. Hormone injections like progesterone mimic the natural increase in progesterone after ovulation. This step is vital for conditioning the endometrium and creating an optimal environment for the embryo. Precision in administering these hormones is critical to improving the chances of a successful pregnancy.
Another significant technique in IVF is intracytoplasmic sperm injection (ICSI). This method involves directly injecting a single sperm into an egg, enhancing the likelihood of fertilization. While not a traditional IVF injection, ICSI is a critical component of the process, illustrating innovative strategies to boost reproductive success.
In summary, IVF injections play a pivotal role in assisted reproductive technology, offering hope to couples facing infertility. From stimulating egg production to coordinating key reproductive processes, these injections significantly improve the likelihood of a successful IVF cycle. Despite some temporary side effects, the potential reward of achieving a pregnancy makes this journey worthwhile. As technology advances, the landscape of IVF injections evolves, providing new opportunities for couples seeking to expand their families.
Why IVF is Done?
Treatment Details
IVF is recommended for patients experiencing infertility, whether primary (inability to conceive naturally) or secondary (inability to conceive after previously having children). Infertility can stem from issues in either the female or male partner or both. Here are some common conditions that may necessitate IVF:
-
Damage or Blockage in the Fallopian Tubes:
The fallopian tubes are where fertilization occurs. If these tubes are damaged or blocked, a mature egg cannot travel to the uterus, preventing embryo implantation.
-
Ovulation Disorders:
Ovulation is the process where a mature egg is released from the ovary. Disorders that disrupt ovulation can result in the absence of an egg during the fertile period, leading to infertility.
-
Endometriosis:
This condition occurs when tissue similar to the uterine lining grows outside the uterus. Affecting 10-15% of women of reproductive age, endometriosis can reduce the number and quality of viable eggs and hinder implantation.
-
Uterine Fibroids:
These non-cancerous tumors can grow in the uterus and vary in size. Hormones influence them and can increase the risk of miscarriage, contributing to infertility.
-
Poor Egg Quality:
Low ovarian reserve can lead to poor egg quality. When a low-quality egg is fertilized, it may not implant successfully, potentially resulting in miscarriage. This is especially common in women over 35.
-
Reduced Fertility in Women Over 40:
Fertility declines with age, particularly after 35. Women over 40 may have significantly lower ovarian reserve and higher miscarriage rates. IVF can help ensure that only genetically healthy embryos are used, reducing health risks.
-
Impaired Sperm Production or Function:
Issues with sperm quality or quantity can prevent fertilization. If sperm count is low or they are not functioning well, infertility can result.
-
The Inability of Sperm to Survive in Cervical Mucus:
Abnormal cervical mucus can hinder sperm motility or even destroy sperm, preventing fertilization.
-
Genetic Diseases:
If one or both partners carry genetic disorders, IVF can help ensure a healthy embryo through preimplantation genetic testing. This allows for the selection of embryos without genetic abnormalities.
-
Unexplained Infertility:
In some cases, the cause of infertility is unclear. IVF can help investigate the patient's health, address any underlying conditions, and proceed with treatment.
IVF offers hope for couples facing various infertility challenges, allowing for tailored treatments that address specific reproductive issues.
What is the IVF Treatment Success Rate?
The success rate of IVF depends on several factors, including:
- Age of the female partner
- Duration of infertility
- Type of infertility (primary or secondary)
- Cause of infertility
- Quality of the sperm, egg, and embryo
- Development of the endometrium
- Luteal phase after transfer
In India, the success rate for IVF ranges from 30% to 35%. Globally, the average success rate is about 40% for younger women, with higher chances of success for those under 35.